The prostate gland synthesizes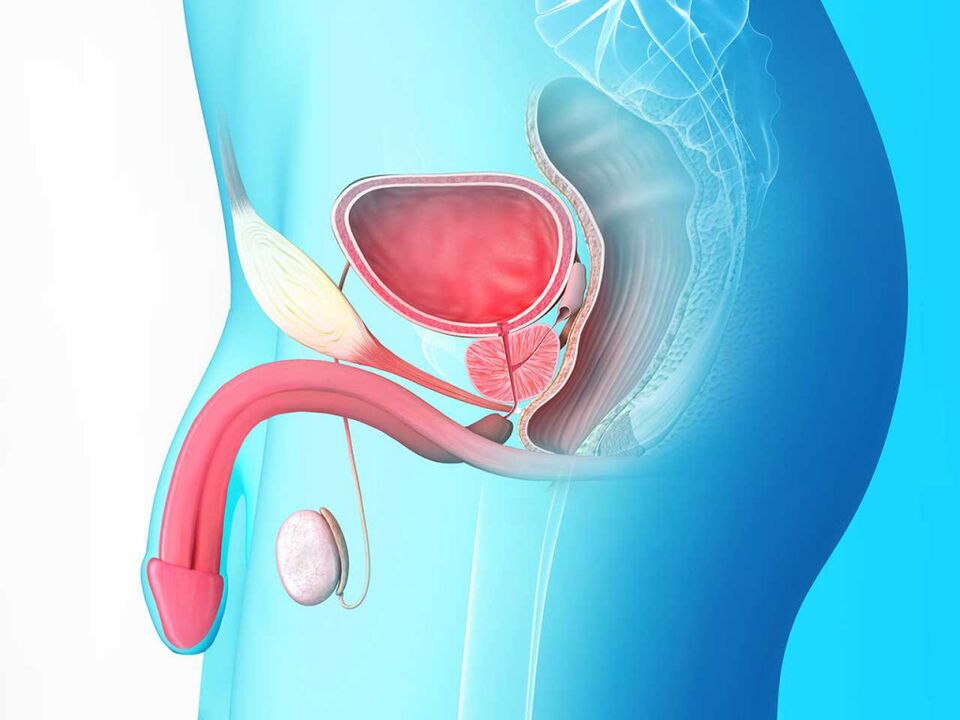 immunoglobulins, regulates sperm viability with the help of a specific secretion, controls the process of urination and ejaculation. Penetration of pathogens into the cavity of this organ provokes prostatitis - an inflammation that occurs in an acute or chronic form.
immunoglobulins, regulates sperm viability with the help of a specific secretion, controls the process of urination and ejaculation. Penetration of pathogens into the cavity of this organ provokes prostatitis - an inflammation that occurs in an acute or chronic form.
Causes and mechanism of disease development
Prostatitis begins with the penetration and reproduction of pathogens in the cavity of the organ. These are extracellular pathogens or their microflora from the surface of the skin or mucous membranes:
- colibacillus;
- Proteus;
- enterococci;
- staphylococcus;
- enterobacteria;
- Pneumococcus.
In the presence of sexually transmitted diseases or infectious diseases of the internal organs, these can penetrate the lumen of the prostate gland:
- pale treponema;
- ureaplasma;
- Trikomona;
- Pseudomonas aeruginosa;
- bacilli and Koch.
In the prostate, pathogenic flora behave ascending from the urethra. Less often - through the bloodstream or with the flow of lymph from the infected organ. A number of provocative factors affect the rate of disease development and the intensity of symptoms:
- abnormalities in the structure of the bladder neck;
- urethral contractions;
- consequences of postoperative catheterization;
- reduced immunity against the background of chronic and systemic diseases, hypothermia, physical overload, hard work;
- violation of blood and lymph flow in the pelvic area;
- deserted or irregular sex life.
An active blood supply and a moist and enclosed environment in the prostate cavity promotes unimpeded reproduction of pathogens. The secretion produced by the gland thickens, its flow is disturbed. Infiltration gradually accumulates in the lumen, inflammation progresses.
The course of acute prostatitis
Primary inflammation usually develops acutely. On average, the patient feels his clinical signs 5-7 days after infection. Its symptoms are vivid, it is impossible not to notice them:
- persistent intense pain in the perineal region, radiating to the scrotum, penis, anus;
- diuresis disorders: frequent, painful urination, false desire, slow current, intermittent urination:
- serous or purulent discharge from the urethra with a sharp unpleasant odor;
- general intoxication: chills, a sharp rise in body temperature, physical weakness, weakness.
Most patients with acute prostatitis have impaired sexual function. Awakening is either completely absent or does not lead to a normal erection and ability to have intercourse. Sperm may contain pus or blood.
The symptoms of bacterial prostatitis depend on the morphological changes and stages of the disease:
- Catarrhal inflammation, which develops early, affects the ducts of the organ and leads to the appearance of deep dull pain. Fever is usually absent, the state of health is generally satisfactory.
- The inflammatory process affects one or both lobes of the gland - follicular prostatitis progresses. Tissues swell, the amount of infiltration into the lumen increases. The pain constantly excludes, increases with movement. Difficulty urinating.
- The parenchymal phase occurs when the entire body of the prostate is affected. The functioning of the bladder and rectum is difficult due to the strong compression of the inflamed, swollen walls of the gland. Pain in the perineum becomes unbearable. Purulent and bloody impurities appear in the urine, body temperature rises to 39 ° C and above.
Delay in treatment provokes chronic disease. Complications are possible: urethral canal blockage, fistulas, abscesses, pyelonephritis, sepsis.
Chronic prostatitis
It develops from an untreated acute, but most often forms as an independent disease. Slow inflammation is caused by an insufficient immune response to the penetration of the infection, a small number of pathogenic microorganisms or the aseptic nature of the disease. In the latter case, the pathology is provoked by the stagnation of secretions, disturbances in the structure of prostate tissue, the permeability of its ducts.
Signs of intoxication and severe pain in chronic bacterial prostatitis occur only with exacerbations. During the latent period, the disease manifests itself with periodic urinary disorders and physical disturbances. The desire to use the toilet is more common at night, after you have been in the cold. Diuresis is sometimes accompanied by a slight burning sensation. Erectile dysfunction is common.
Chronic prostatitis can last for years with occasional beatings. A long-term course leads to the formation of fibrous areas in the parenchyma, provokes the development of impotence, infertility and oncological tumors.
How to diagnose and treat prostatitis
If you suspect the development of prostate inflammation, you should contact a urologist. The presumed diagnosis is confirmed by bacterial culture of glandular secretion. If it is impossible to get it, examine a stain from the urethra, urine sample, seminal fluid. In addition to bacterial inoculation, blood and urine tests are performed, prostate ultrasound is performed.
Treatment of acute infectious prostatitis is performed in a clinical setting in the Department of Urology.
- The main focus is on suppressing the pathogen, relieving inflammation, and preventing complications. The patient is prescribed a course of antibiotics. Injections of drugs from the groups of tetracyclines, cephalosporins, fluoroquinolones or penicillins are used, depending on the infection that caused the disease. Duration of therapy: from a few days to 2-4 weeks.
- To restore urinary function and relieve acute symptoms, muscle relaxants, anti-inflammatory pain relievers, and antispasmodics have been comprehensively prescribed.
- Specific therapy is supplemented with preparations of vitamins and minerals, immunomodulators.
In the early stages, uncomplicated inflammation heals completely.
Chronic prostatitis does not require hospitalization. The patient undergoes a course of antibiotic therapy at home, respecting the necessary restrictions.
In parallel, it is necessary to undergo a course of treatment for possible provocative diseases: bronchitis, pyelonephritis, cholecystitis, genitourinary infections.
The main treatment without deterioration is supplemented by physiotherapeutic methods: ultrasound procedures, magnetotherapy, laser exposure.
During the therapy period, alcohol, hot spices, marinades, pickles, fatty, canned and smoked foods should be excluded. It is recommended to include in the diet fresh herbs, vegetables, nuts, fish, lean meats.
The success of treatment of the chronic form in each case depends on the duration of the disease, the existing damage to organic tissue, concomitant disorders in the functioning of the kidneys and bladder.



























